
Looking for something specific? Jump to the content you need right away!
Also referred to as varicosities, varicose veins are swollen, twisted veins that may bulge underneath the skin. Most often, varicose veins appear as swollen and raised veins with a bluish-purple or slightly red color. Typically, varicose veins are painful as well. Varicose veins occur when the veins’ valves become damaged or don’t function properly, causing blood to leak back through the valves and pool in the veins. As the veins overfill with blood, they become enlarged and dilated. Although any vein can become a varicose vein, the most common place where varicose veins form is in the lower legs because of the increased pressure that standing up and walking around can put on the veins. The severity of varicose veins can range from strictly cosmetic to more serious health complications. Depending on the severity of the case, there is a variety of at-home treatments and medical procedures available for addressing varicose veins. Find out more about bleeding varicose veins.
We believe it’s important for patients to understand how unhealthy veins work. However, it’s just as important to understand how veins work when they’re healthy. Your body relies on a complex network of vessels to keep blood flowing throughout the body. While arteries deliver oxygenated blood to muscles and organs, veins are responsible for pumping the deoxygenated blood back to the heart. When leg muscles contract, vein valves open, and blood is squeezed up the vein. When leg muscles relax, the valves close, and this prevents blood from leaking backward in the vein. Strong, healthy valves are equipped to safely hold blood in place until the next time muscles contract.
Let’s compare healthy veins to unhealthy ones. Whereas healthy veins have strong walls and valves, damaged ones do not. Damaged veins do not function properly and blood can leak and pool causing them to swell. This means that they’re no longer able to fully close, allowing blood to leak back through the valve when muscles relax — and forcing the blood to reroute to the nearest healthy valve. But the extra pressure becomes too much for that once-healthy valve. The valves below it are impacted as well. Blood pools in the vein instead of moving back to the heart as it should, and as a result, varicose veins can occur.
As previously mentioned, your body relies on a large network of veins to carry blood from the body back to the heart. There are several types of veins that work together to make this happen! Superficial veins are close to the surface of the body and drain into deep veins. The deep veins then carry blood back to the heart through the inferior vena cava. This is the body’s largest vein! Lastly, there are perforating veins, which help transport blood from the superficial veins to the deep veins.
Although 1 in 5 adults get varicose veins at some point in their lives, many do not know the root cause of varicose veins or how to treat them. Despite the fact that varicose veins are quite common, many people are also unaware of how veins are meant to function at their healthiest. Understanding the basics of veins allows you to be better prepared to avoid varicose veins and address them if they become an issue. This ultimate guide to understanding varicose veins will cover everything you need to know from how to identify unhealthy veins to varicose vein treatment options. If you’ve ever wondered whether your veins are as healthy as they should be, this article is for you.
At Central Florida Vein and Vascular Center, we are dedicated to educating our clients. We’re happy to answer any questions you have, and we want to ensure that you know as much about your vein health as possible. Keep reading to learn more about the different types of veins, the important roles they play in your body, the stages of varicose veins, common misconceptions, risk factors, and how varicose veins can form.
There is a wide variety of tests a medical professional can use to discern whether or not a patient has varicose veins. Below are the options available for diagnosing varicose veins:
Numerous variables, such as a sedentary lifestyle, weight gain, hormonal changes or a family history of venous insufficiency can impact the likelihood of developing varicose veins. A full review of a patient’s medical history can provide a specialist with the information they need to diagnose a venous issue and any related health concerns.
During a physical examination, a physician can look at the legs and feet for signs of varicose veins, such as skin discoloration, tenderness, swelling or ulcers. Getting the patient to move around a bit can also be an effective way to check circulation and proper vein functioning.
For a more in-depth look at vein health, there are a few imaging tests a patient can undergo. These three tests may produce more conclusive results:

When it comes to treating varicose veins, addressing the problem earlier is always better. Delaying the treatment of varicose veins can allow symptoms to worsen and more serious medical concerns to develop. To avoid further health complications due to varicose veins, it is important to see a vein specialist for proper diagnosis and treatment as quickly as possible. The exact procedures for how to cure vein pain in legs will depend on the severity of the vein damage. Less severe cases of varicose veins may be effectively managed with the right self-care practices and strategies for minimizing symptoms. For varicose veins that need more than at-home solutions, there are a variety of varicose vein treatment options a vein specialist can recommend that are minimally invasive and oftentimes covered under medical insurance. Most of these procedures involve little to no pain and allow patients to resume normal activities within one to two days.
Top treatment options for varicose veins include:
There are multiple self-care techniques to mitigate the symptoms that typically go along with varicose veins. For instance, avoiding tight clothing and standing or sitting for extended periods of time can help reduce the pain caused by varicose veins while preventing them from getting worse. Additionally, elevating the legs, exercising regularly and losing weight can lessen varicose vein symptoms.
Compression socks apply gradual amounts of pressure to the legs, which helps guide blood flow up the legs. Although compression socks are not a cure for varicose veins, wearing them to assist blood flow can relieve the pain or heaviness in the legs caused by varicose veins. Compression socks can also help keep blood pressure steady and prevent or manage spider veins.
For more serious cases of varicose veins or a varicose vein emergency, the damaged veins may need to be resolved. The following options of medical treatment for varicose veins offer minimally invasive ways to effectively eliminate unhealthy veins.

Although many people believe vein treatment is not included in their insurance coverage because it is a cosmetic concern, varicose vein treatment is recognized as a medical necessity by insurance providers. Because the root cause of varicose veins — venous insufficiency — is a serious health problem, varicose vein treatment is covered by medical insurance. The Centers for Medicare and Medicaid Services (CMS), along with most private insurers, have approved coverage of varicose vein care procedures because the symptoms varicose veins can cause directly interfere with a patient’s quality of life. On the other hand, spider vein treatment addresses superficial veins, which are more cosmetic and not included by most insurance plans.
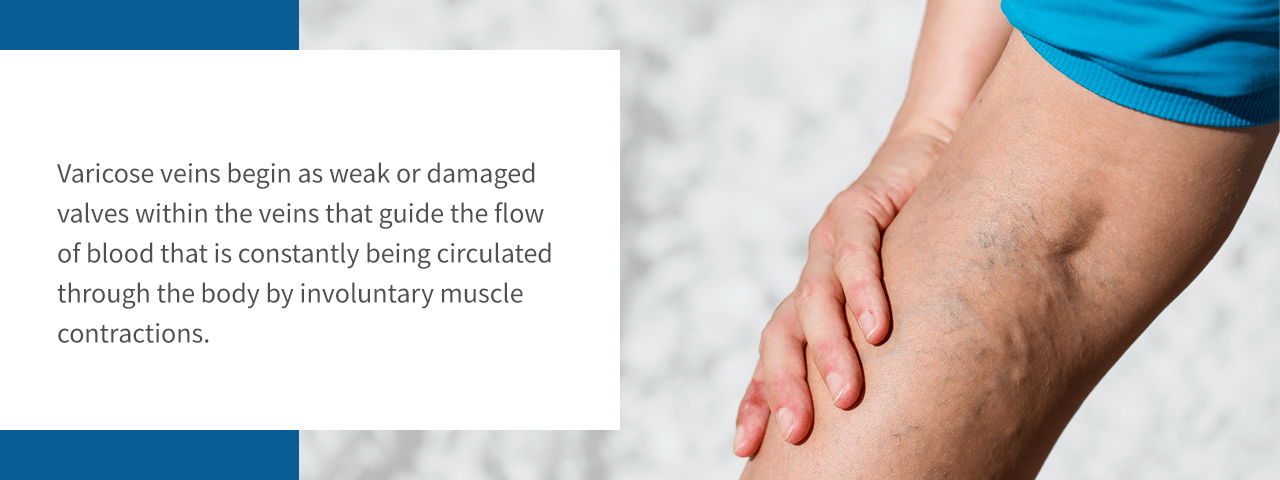
How do varicose veins start? Essentially, varicose veins begin as improperly functioning valves within the veins that guide the flow of blood that is constantly being circulated through the body by involuntary muscle contractions. The tiny valves located in the veins have to open and allow blood to flow toward the heart, then close to prevent blood from flowing backward. When these valves don’t function properly, blood can flow backward and start to pool in the vein. This buildup of blood forces the vein to stretch, twist and enlarge. These contorted veins are known as varicose veins. Because the veins in the legs have to work against gravity when returning blood to the heart, varicose veins in quads, calves and other parts of the leg are the most common types of varicose veins. Along with the stress of fighting gravity, there are a wide variety of other factors that lead to varicose veins, including:
See other habits that cause varicose veins.
Despite how common varicose veins are, most people believe many myths about varicose veins, from what causes them to how to deal with them. Some of this misinformation is relatively harmless, such as the misconception that wearing high heels leads to varicose veins. Although wearing heels every day can gradually damage venous health by limiting blood movement, occasionally wearing heels is perfectly acceptable. Some varicose vein misconceptions are more dangerous. For instance, many people think no special training is required for treating a chronic venous disease like varicose veins. On the contrary, an unqualified practitioner will not know how to appropriately diagnose or treat varicose veins. To help you discern varicose vein fact from fiction, we’ll address three of the most widely propagated varicose vein rumors:
If left untreated, this form of venous insufficiency risks becoming a worse health concern. Sometimes veins can leak and create an ulcer, and in the worst-case scenario, blood clots can form in areas of the vein where blood moves too slowly or not at all. This clot can travel to the lungs and cause a pulmonary embolism. Learn about what happens if varicose veins are untreated.
Many varicose veins are benign and do not lead to serious health issues. Some people with varicose veins do not suffer any symptoms, making varicose veins a purely cosmetic concern. In other cases, varicose veins can cause discomfort, aching pain or be a warning of an underlying problem within the body’s circulatory system. Because varicose veins are a result of damaged vein valves, they can make it more difficult for the body to circulate blood properly. A lack of blood flow can lead to larger health issues. Learning to recognize the more concerning signs of unhealthy veins is an important part of knowing when to worry about varicose veins and when to see a vein specialist.
More serious varicose veins complications include:
Although varicose veins can develop into a more significant health condition, they are not an indication of heart disease. Because the heart relies on arteries, rather than veins, for its blood supply, problematic veins are generally not linked to heart health. Read about bleeding varicose veins.
Although there is no guaranteed way of completely preventing varicose veins, there are some healthy practices that can decrease the risk of developing them. Adopting habits that help boost circulation and build muscle tone can reduce the chances of varicose veins forming as well as minimize the discomfort often caused by varicose veins.
To avoid varicose veins, follow these guidelines:
At Central Florida Vein and Vascular Center, we are proud to work with the finest vein specialists in Kissimmee. We offer a full spectrum of the latest services in vein care, and we take the time to create a treatment plan that is fully customized to your individual needs. We stay up to date with new trends and focus on providing the highest quality of patient care as our top priority. It is also common to have questions, and we are happy to talk through them with you. Contact us today at 407-545-3385 or 352-658-5547 to find out how our treatments can change your life.
Advice from Vein Specialists
How to Choose a Specialist
Varicose Veins & Insurance
Vein & Vascular Basics
Varicose Vein Basics
Varicose Veins – Causes & Prevention
Diagnosing Varicose Veins
Risk Factors, Complications, Warning Signs
Symptoms – Bleeding, Itching, Skin Issues, Bulging, Clots & Ulcers
Varicose Veins & Lifestyle Information
Managing Varicose Veins – Sleep, Walking, Footwear, Pregnancy, More
Varicose Vein Treatment
Post – Treatment
What You Should Know About Home Remedies