Visible leg veins can impact more than your appearance. Varicose veins in the legs point toward a more severe underlying problem called venous insufficiency. The cause of venous insufficiency is weakened vein valves. When chronic venous insufficiency occurs, leg veins could become severely damaged, which is why diagnosing and treating any venous conditions as early as possible is crucial.
If you’re starting to notice varicose veins, spider veins, swelling, heaviness or aching in your legs, this ultimate guide to damaged leg veins will help you determine the right treatment plan for your veins. This article will cover the various types of visible leg veins, symptoms of spider veins and treatment options, along with what to expect during your vein specialist appointment.
Most commonly, venous issues occur in the legs because vein valves located in your legs have weakened to the point where they can no longer allow proper blood flow. The weakening causes venous blood to collect in weak veins making them work as vein valves located elsewhere in your body to circulate blood. Because veins are responsible for returning the blood to the heart, leg veins must fight against gravity to pump blood upward. The muscles in the feet and calves assist this process by squeezing the veins to help push the blood along.
Over time, the added pressure of pumping blood against the weight of gravity can start to wear down the vein valves within the legs’ veins. Once the vein valves become weakened or damaged and stop functioning at their highest capacity, blood can begin to pool in the leg, resulting in pain, swelling and any number of venous conditions.
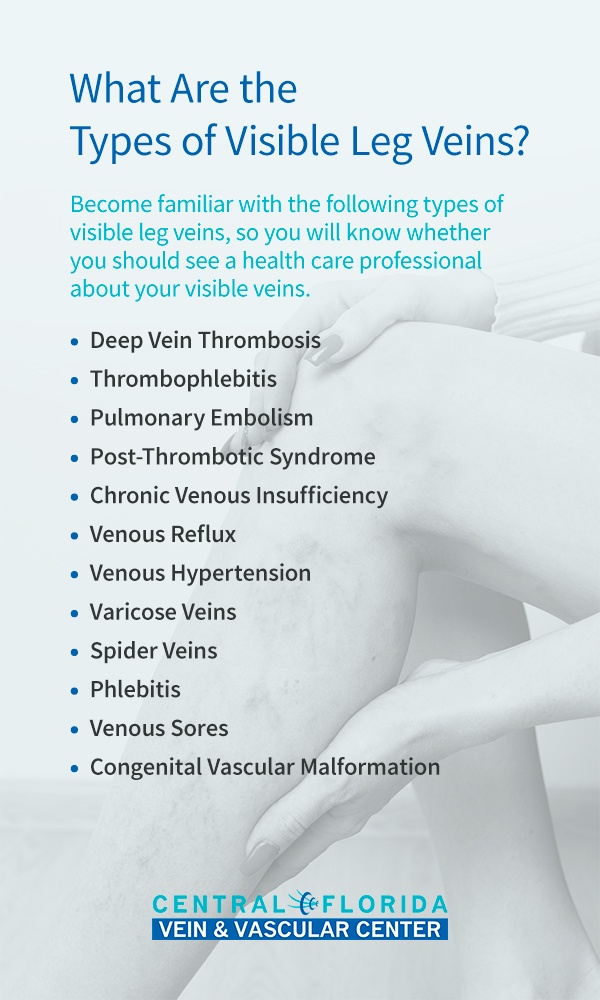
Because the appearance of damaged veins in legs links with various venous conditions and health concerns, it is essential to accurately determine the cause of visible leg veins as early as possible. While some vein complications are purely cosmetic and are easy to address through self-care or minimally invasive treatments, other venous conditions can lead to severe health threats.
Become familiar with the following types of visible leg veins, so you will know whether you should see a health care professional about your visible veins.
Deep vein thrombosis is the official medical term for a blood clot. A blood clot forms when blood moves too slowly through the veins, typically due to damaged or weakened valves within the veins that make them less capable of pushing blood. As a result, blood begins to pool in the vein, leading to a blood clot.
Because deep veins are responsible for transporting the majority of our blood back to the heart, you should have this condition addressed as soon as possible. Keep an eye out for the most common sign and symptoms of deep vein thrombosis, including swelling, leg pain, red or discolored skin around the leg vein or a feeling of warmth within the affected leg.
Similar to deep vein thrombosis, thrombophlebitis is painful hardness in a superficial vein caused by a blood clot within the vein with inadequate blood flow. However, thrombophlebitis symptoms and swelling tend to be less concerning than deep vein thrombosis because they occur in superficial veins. If left untreated, thrombophlebitis could progress into deep vein thrombosis, a much more severe health condition.
A pulmonary embolism occurs when a blood clot separates itself from a deep vein and moves into a large vein in the lung. This can cause a tremendous strain on the heart, causing it to fail and it is a life-threatening medical condition. People with a pulmonary embolism should call 911 immediately if they experience difficulties breathing or begin to cough up blood.
In some cases, the painful and irritating symptoms of deep vein thrombosis persist even after treatment. This condition is known as post-thrombotic syndrome. Post-thrombotic syndrome usually occursas a result of the scarring in the wall of the deep vein from the blood clot, making the deep vein not function properly.
In some cases, the painful and irritating symptoms of deep vein thrombosis persist even after treatment. This condition is known as post-thrombotic syndrome. Post-thrombotic syndrome usually occursas a result of the scarring in the wall of the deep vein from the blood clot, making the deep vein not function properly.
Venous insufficiency refers to when the walls or the valves within the leg’s veins do not work sufficiently, making it difficult for blood to flow smoothly from the legs back to the heart. When this condition becomes a long-term problem, it is chronic venous insufficiency (CVI), which could result in blood pooling in the damaged veins.
Causes of chronic venous insufficiency include vein valve damage from pregnancy, obesity, jobs where you stand a long time, deep vein thrombosis, family history and a lack of exercise. Treating CVI as early as possible is imperative because the disease’s severity worsens as it progresses. If left untreated, the pressure and swelling that accompany CVI can build up in the leg until the varicose veins, swelling and possible ulceration develop.
Damaged venous valves that no longer function properly can result in the reversal of blood through the valves when people with this condition are sitting or standing. This condition, known as venous reflux, most often occurs when vein valves become weakened due to genetic influences, multiple pregnancies, blood clots or high blood pressure.
Increased pressure inside the veins can lead to venous hypertension. Persistent venous hypertension is known as chronic venous hypertension, which often stems from CVI and blood leaking backward through the vein’s valves. Chronic venous hypertension could also result from an obstruction in the veins due to blood clotting, obesity or the compression of pelvic or abdominal veins.
Often, venous hypertension symptoms include swelling, tenderness, pain, skin changes or even venous leg ulcers.
Varicose veins are swollen, bulging, twisted veins that have a darker appearance underneath the skin. These inflamed veins can form when the valves within them become damaged or weakened and blood leaks back through the valves, pooling in the veins and causing them to swell. Though varicose veins can be unsightly, they are always unhealthy for the legs. they can lead to more severe health conditions, such as deep vein thrombosis, CVI, venous reflux and pulmonary embolism.
Spider veins are thinner than varicose veins and appear as small, blue, web-like veins just under the skin’s surface. Though this condition relates to venous insufficiency, spider veins are not as severe as varicose veins and do not typically bulge or swell like varicose veins. While anyone can develop these branch-like veins, aging, genetics, pregnancy, trauma and sun damage are the leading causes of spider veins.
Phlebitis is the general term that refers to vein inflammation. Phlebitis can occur with or without a blood clot and can affect either deep or superficial veins. When a blood clot is not present, the swelling is typically due to trauma to the vein. For example, an intravenous catheter could be the cause of phlebitis.
Also known as venous ulcers, venous sores occur when the amount of pressure in the veins builds up over a long period and breaks down the leg’s healthy tissue. Approximately 85% of these leg ulcers are attributable to vein complications. Specifically, venous reflux could result in venous ulcers. Similarly, seemingly harmless varicose veins can lead to leg ulcers if not treated properly and promptly.
This term applies to any defective vein condition someone has from birth, which is extremely rare. For example, someone might be born with veins that lack valves. Congenital vascular malformation also includes birthmarks that appear as a cluster of veins close to the skin’s surface.

While spider veins are generally the least concerning form of venous insufficiency, they are still a result of weakened or damaged valves within the veins. If you have spider veins, you and your doctor should monitor them closely to ensure they do not develop into a more severe health issue, such as varicose veins or deep vein thrombosis.
If you think you might have spider veins, consider the three most crucial factors of the venous condition below.
While spider veins’ coloring can range from blue to purple to even slightly reddish hues, the web-like veins are always small and look as thin as thread. As opposed to bulging varicose veins, spider veins tend to be flat or only slightly raised. Spider veins are often in the legs, but chest, facial and hand veins might also develop into spider veins.
While many superficial spider veins are a cosmetic concern, more severe cases of spider veins can interfere with your quality of life since they burn, itch, and sting. It’s essential to recognize that spider veins that begin as milder cases can quickly worsen when left untreated. Specifically, spider veins that come with symptoms like pain and swelling are more likely to progress toward venous ulcers or blood clots.
Even if you think your spider veins are relatively mild, it is always smart to see a vein specialist to ensure the spider veins do not indicate an underlying vein problem. If your spider veins link to a deeper vein problem, there is no need for distress. For most vein conditions, treatment is easy and minimally invasive, so most patients can even return to work the day after treatment.
Though spider veins may not feel any different from regular veins, some spider veins can cause pain and discomfort. More severe spider vein cases may be sore or tender to the touch. In rare cases, spider veins may even cause a burning sensation. Worsening discomfort surrounding spider veins is often a sign of a more severe venous condition, in which case you should consult with a vein specialist as soon as possible.
Depending on how severe your visible leg veins are, you can choose from an array of at-home treatment options and medical procedures. This section will discuss the range of self-care strategies and medical treatments available to you.
Some self-care measures can be an effective leg vein treatment for mild venous conditions, such as spider veins. Try these five at-home treatments for managing your venous symptoms.
Maintain a healthy weight
Wear compression hose if standing a long period of time or traveling
Compression stockings assist the leg veins by applying steady pressure to help pump the blood back toward the heart. The increased circulation produced by this pressure helps minimize the swelling and pain associated with varicose veins by gently pushing pooled blood back up the leg. Compression socks can also help reduce the risk of developing a blood clot.
Compression socks are available in various sizes and compression levels, so you can be sure to find the right fit for your feet and condition. A specialist can determine which type of compression stocking will be the most beneficial for you.
While self-care methods can be effective solutions for mild spider vein treatment, more severe venous issues may need further medical attention. If you have varicose veins or another vein condition, consider these minimally invasive techniques to treat it successfully.
· Sclerotherapy: In sclerotherapy, a doctor injects a solution into the affected vein, which scars the vein and forces blood to flow through healthier veins instead. The body then gradually absorbs the scarred vein. Variations of sclerotherapy include veinlite sclerotherapy, which uses a light placed on the skin to transilluminate the vein so the doctor can place the needle, and ultrasound-guided foam sclerotherapy, which relies on ultrasound technology to locate the affected vein.
If your venous condition has progressed to the point of needing professional treatment, here is what you can expect from a visit to your vein specialist.
Before making a final diagnosis, your doctor will review your medical history and conduct a physical exam. The physical exam will check the blood flow in your legs and determine whether leg vein treatment is right for you. The physical exam will include a diagnostic vascular ultrasound, which uses sound waves to allow your doctor to see how well the vein valves in your legs are working to circulate your blood.
After going over the vascular ultrasound results and accounting for your symptoms, your doctor will make a diagnosis.
Once you have received a diagnosis, your vein specialist will present you with treatment options. Depending on your condition’s severity, your treatment choices could range from at-home solutions to minimally invasive procedures. Your vein specialist should review all the treatment plans available to you and recommend the best course of action to produce results while reducing side effects.
Before making any final treatment decisions, be sure to ask your doctor these seven essential questions:

If you’re experiencing any form of venous insufficiency, visit the vein experts at Central Florida Vein and Vascular Center. As one of Central Florida’s top dedicated vein care facilities, Central Florida Vein and Vascular Center offers highly specialized care and a range of minimally invasive vein therapies. Because all of our procedures are minimally invasive, you can return to light-duty work immediately following treatment.
To learn more about your treatment options or to schedule an appointment with a specialist, contact Central Florida Vein and Vascular Center today.